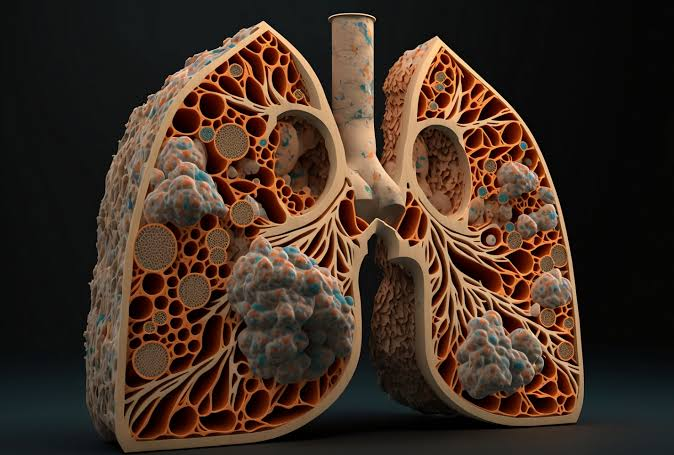
Interstitial Lung Disease (ILD)
Interstitial Lung Disease (ILD) refers to a group of disorders characterized by inflammation and scarring (fibrosis) of the lung tissue, particularly the interstitium—the area of tissue surrounding the alveoli (air sacs). These diseases impact the lung’s ability to transfer oxygen into the bloodstream, leading to breathing difficulties and a decline in lung function.
How serious is interstitial lung disease?
The seriousness of interstitial lung disease (ILD) can vary depending on the specific type. Some forms of ILD may be mild, while others can be very severe. Generally, ILDs tend to cause irreversible lung damage. The most severe cases are progressive, meaning the condition gradually worsens over time.
Signs
Common signs of ILD include:
- Persistent dry cough
- Shortness of breath, especially with exertion
- Fatigue and general malaise
- Unexplained weight loss
- Clubbing of the fingers (widening and rounding of the tips of the fingers)
Symptoms
Symptoms of ILD can vary depending on the specific type and severity of the disease. Common symptoms include:
- Chronic cough: A dry, persistent cough that does not go away.
- Breathlessness: Difficulty breathing or shortness of breath, particularly during physical activities.
- Fatigue: Feeling unusually tired or weak.
- Chest discomfort: Discomfort or a feeling of tightness in the chest.
- Decreased exercise tolerance: Reduced ability to perform physical activities due to breathing difficulties.
Types
ILD encompasses various conditions, including:
- Idiopathic Pulmonary Fibrosis (IPF): A common and severe form of ILD with unknown cause, leading to progressive lung scarring.
- Non-Specific Interstitial Pneumonia (NSIP): Characterized by inflammation and fibrosis with a somewhat better prognosis than IPF.
- Cryptogenic Organizing Pneumonia (COP): Involves inflammation and scarring of the lungs, often responding well to treatment.
- Hypersensitivity Pneumonitis (HP): Caused by an allergic reaction to inhaled organic dust, leading to inflammation and scarring.
- Sarcoidosis: An inflammatory disease that can affect the lungs, characterized by granulomas (small clusters of inflammatory cells).
- Collagen Vascular Diseases: Such as systemic sclerosis or rheumatoid arthritis, which can involve ILD as part of their manifestations.
Diagnosis
Diagnosis of ILD involves several steps:
- Medical History and Physical Exam: Review of symptoms, medical history, and physical examination to assess lung function and overall health.
- Imaging Tests:
- Chest X-ray: Provides an initial view of lung abnormalities.
- High-Resolution Computed Tomography (HRCT): Offers detailed images to identify specific patterns of lung damage.
- Pulmonary Function Tests (PFTs): Measures lung capacity and function to assess the extent of impairment.
- Bronchoscopy: Allows visualization of the airways and, if necessary, biopsy samples for further examination.
- Lung Biopsy: Obtaining a sample of lung tissue for pathological analysis to confirm the diagnosis and type of ILD.
Treatment
Medications
- Corticosteroids: Reduce inflammation and can improve symptoms.
- Immunosuppressants: Drugs like azathioprine or mycophenolate mofetil to modulate the immune response.
- Antifibrotic Agents: Such as pirfenidone and nintedanib, specifically for conditions like IPF to slow down fibrosis.
Lifestyle and Supportive Therapies
- Oxygen Therapy: To provide supplemental oxygen for patients with low blood oxygen levels.
- Pulmonary Rehabilitation: Includes exercise training and education to improve physical functioning and quality of life.
- Vaccinations: Influenza and pneumonia vaccines to prevent respiratory infections.
Surgical Treatments
- Lung Transplantation: Considered for advanced cases of ILD when other treatments are no longer effective.
Prevention
How can I reduce my risk of interstitial lung disease?
While many causes of interstitial lung disease (ILD) cannot be prevented, you can lower your risk by managing underlying conditions and avoiding exposure to harmful substances:
- Protect Yourself: Use a respirator or mask when working with harmful materials such as asbestos, metal dust, or chemicals.
- Avoid Allergens: Wear a respirator when exposed to substances that may trigger chronic allergic reactions, including hay, grain, bird droppings, feathers, and certain heating and cooling systems.
- Manage Existing Conditions: If you have a connective tissue disease or sarcoidosis, consult your healthcare provider about managing your condition to reduce the risk of developing ILD.
- Avoid Smoking: Refrain from smoking or seek help to quit if you currently smoke.
FAQs
The exact cause of ILD can vary depending on the type, with some cases being idiopathic (of unknown cause) and others related to specific conditions such as autoimmune diseases, environmental exposures, or genetic factors.
Yes, many forms of ILD are progressive, meaning they can worsen over time. Early diagnosis and treatment can help manage symptoms and slow the progression.
Management involves a combination of medications, lifestyle changes, and supportive therapies. In severe cases, lung transplantation may be considered.
There is no universal cure for ILD. Treatment focuses on managing symptoms, improving quality of life, and slowing disease progression.
Engaging in pulmonary rehabilitation, maintaining a healthy lifestyle, adhering to prescribed treatments, and avoiding exposure to lung irritants can improve quality of life.
Conclusion
Bronchoscopy is a valuable tool in diagnosing and treating various respiratory conditions. If you have concerns or symptoms that may require a bronchoscopy, consult with your healthcare provider to determine if this procedure is appropriate for you.